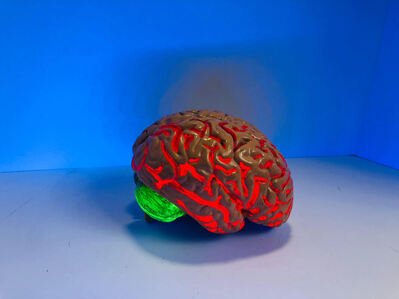
The Injured Pre-Frontal Cortex
In our previous blog, we discussed the brain and its various characters. As a refresher, the brain is comprised of two keys players: the limbic system and the pre-frontal cortex. The limbic system is the “animal” part of our brain; it is where our emotions originate and houses our fight-or-flight response system. The limbic system sits deep down in the center of our brain and is surrounded by the outer cortical surface of the brain called the cortex. The cortex is comprised of five major lobes: the frontal, parietal, temporal, occipital, and cerebellar areas. Each of these lobes play a distinct role in human function, but the frontal lobe, arguably, may be the most important in terms of human consciousness.
The frontal lobe is segmented into a handful of definitive areas, one of which is called the prefrontal cortex (PFC). Sitting at the most anterior portion of the frontal lobe in our forehead region, the PFC is responsible for a myriad of functions. At the top of the list, the PFC is mainly in charge of executive function (Siddiqui, 2008). Executive function includes many of the everyday tasks we need to function in society, such as an ability to pay attention, retain new information, communicate with others, and engage in goal-directed behaviors. The PFC functions at peak performance when we are listening to a teacher explain a new concept, brainstorming new ideas with our boss at work, or planning a family vacation. The PFC has also been linked to each individual’s overall intelligence level, as many IQ tests challenge the PFC’s responsibilities directly.
As mentioned in the first edition of this blog, the PFC interacts with the limbic system on a constant basis. The PFC acts as the gatekeeper to our emotionally charged limbic system and ensures our emotional impulses are kept in check and our needs are being met. However, this delicate communication system can be severely compromised when the PFC becomes injured.
An injury to the PFC can come about in hundreds of different ways. Perhaps of the most famous brain injuries every recorded occurred in the fall of 1848 (Garcia-Molina, 2010). Phineas Gage was born in New Hampshire and found work as a railroad constructor, taking him all the way to the western coasts of California. At the age of 25, a tragic accident occurred. Phineas Gage was standing over an area of rail line that exploded, causing an iron tamping rod to rocket out of the ground straight upwards into the left side of Phineas’ skull. The rod penetrated through his left jaw, traveled behind his left eye socket, and exited out of the top of his left frontal lobe. Shockingly, he survived, and lived 12 more years before dying of an epileptic seizure. However, those 12 years were marked by extreme personality changes for Phineas, and this dramatic injury changed the medical community’s understanding of the significance of the PFC in a person’s neuropsychological function.
While the story of Phineas Gage is severe, many injuries to the frontal lobe often result from everyday occurrences. In the United States, motor vehicle accidents and slip-and-fall accidents account for over half of all traumatic brain injury (TBI) hospitalizations (Center for Disease Control and Prevention, 2021).
In addition, concussions and TBI’s from sport-related accidents are also becoming increasingly concerning. Both children/adolescent and professional sports such as football, hockey, lacrosse, and soccer are gaining national media attention for athletes suffering from long-term head injury symptoms.
So, what happens exactly when the frontal lobe is injured?
The PFC sits in the foremost portion of the frontal lobe, directly behind the bones of our forehead. There is little space between the PFC and these skull bones. The PFC is suspended in the skull and its’ only protection from the skull bones are thin layers of tissue and membrane. During a head impact event, the delicate tissue of the PFC can be jostled back and forth, causing it to come into contact with the skull bones. Next, the brain ricochets backwards, and this forward and backward momentum continues until the brain reaches a resting point.
Imagine a piece of Jello sitting on a plate: as the plate moves back and forth, the Jello jiggles front to back and side to side. Even once the plate becomes still, there may still be subtle movements of the Jello due to physics and the properties of inertia.
While the brain is not quite Jello consistency, it is this movement that often results in the traditional symptoms we associate with concussions and TBIs.
The U.S. Department of Veteran’s Affairs and Department of Defense defines and classifies severity of TBI using the following criteria: loss of consciousness, memory loss, altered mental state, neurological deficits, Glasgow Coma Scale, and imaging results. Common symptoms of mild TBI include:
Difficulty focusing and concentrating
Trouble paying attention or staying on task
Headaches
Fatigue
Increased irritability or anger management problems
Increased emotional susceptibility
Personality changes
In addition, depending upon the severity of injury, other parts of the brain’s cortex can become injured, resulting in additional symptoms that are often difficult to diagnose at face value.
Injury to the PFC can greatly alter a person’s ability to function in everyday society. For many, a TBI diagnosis can have lifelong impacts and depending upon a person’s specific recovery, may or may not improve over time. However, there are many therapeutic options for TBI treatment.
Perhaps one of the most helpful interventions can simply be understanding what a brain injury is and how the PFC changes after an injury. Through the use of psychoeducation, we can begin to better understand how our PFC functions post-injury and in turn, make appropriate accommodations at work, school, and home. As we learn to better understand how the PFC functions and what it needs for recovery, we can learn to give ourselves grace and the time it often takes to adapt to a new way of functioning.
Living with a brain injury is challenging, but with the right resources and support from loved ones and health care providers, thriving with a brain injury is possible.
The office of Hilary Morris, LPC provides psychological services and trauma therapy for those struggling with emotional symptoms following TBI or concussion. They provide psychotherapy to help clients learn to gain control over episodes of anxiety or panic. Their clients integrate changes into their daily life and make peace with their brain injury recovery process.
For more information on brain injury and brain injury recovery, please refer to these organizations advocating for TBI-patient care:
Brain Injury Association of America (https://www.biausa.org/)
Brain Injury Hope Foundation (https://www.braininjuryhopefoundation.org/)
US Department of Veterans Affairs (https://www.mentalhealth.va.gov/tbi/)
Centers for Disease Control and Prevention (https://www.cdc.gov/traumaticbraininjury/get_the_facts.html)